Gestational Trophoblastic Disease – Molar Pregnancy
Question: What is a Molar Pregnancy?
Answer: A molar pregnancy, also known as hydatidiform mole, is a rare type of conception occurring in about 1 in every 600 pregnancies. A molar pregnancy is an abnormal pregnancy that begins at the time of conception when the sperm and the egg join together. This type of conception has excessive development of the cells that form the placenta (also known as the ‘afterbirth’) and a molar pregnancy has little or no fetal (baby) development.
There are two types of molar pregnancy known as complete hydatidiform mole (CHM) and partial hydatidiform mole (PHM). These two types of molar pregnancy differ in their genetic makeup and development.
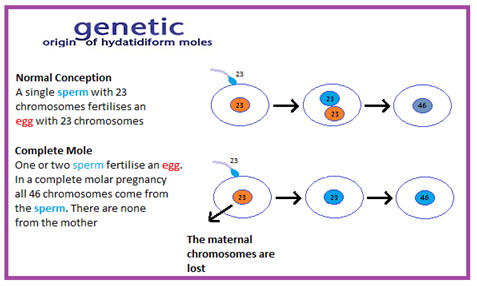
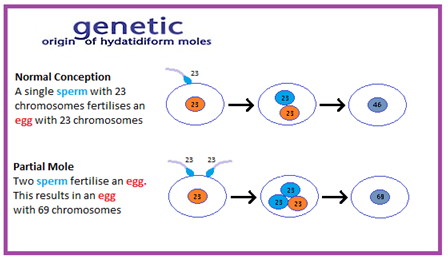
Question: What happens in a normal conception?
Answer: In a normal conception an egg from the mother has 23 chromosomes (these are strands of DNA that contain our genes). This egg is fertilised by the father’s sperm that also has 23 chromosomes which join up to create a baby (fetus) made up of 46 chromosomes. Two of these 46 chromosomes are what we call the sex chromosomes (one from each parent)
Complete molar pregnancy (CHM)
In complete molar pregnancy the genetic information (chromosomes) has been inactivated or lost from the mother’s egg. The “empty” egg is fertilised by the father’s sperm so there are only 23 chromosomes present. In normal conception there should be 46 chromosomes in a fertilised egg but in this situation duplication of the father’s chromosomes (including the two sex chromosomes) occurs producing the normal number of chromosomes leading to 46 chromosomes – but all from the father. A baby cannot develop as there is no genetic input from the mother. However, the cells that form the placenta will grow rapidly and your pregnancy test will be positive. In addition, you may have physical symptoms associated with normal pregnancy for example breast tenderness, nausea and vomiting. This happens because the over-production of these placental cells will produce high levels of the pregnancy hormone (hCG). Because of the growth of the abnormal placenta women with CHM often present with early pregnancy bleeding and the diagnosis can usually be suspected on ultrasound scan.
Partial Molar Pregnancy (PHM)
In partial molar pregnancy two sperm fertilise a normal egg leading to one set of chromosomes from the mother and two sets from the father – a total of 69 chromosomes (with 3 sex chromosomes). Again there is an imbalance of chromosomes but it differs from CHM as there can be evidence of some fetal development. These pregnancies almost always end in miscarriage. The majority of partial moles present with early pregnancy bleeding but the ultrasound scan is not usually diagnostic and the diagnosis is only made when laboratory examination of the miscarriage tissue has taken place.
Question: How is molar pregnancy diagnosed?
Answer: An ultrasound scan may indicate that a complete molar pregnancy (CHM) is present and you will be admitted to hospital for a surgical procedure called an ERPC – evacuation of the retained products of conception. This procedure is necessary to remove the molar tissue. This is because there is a risk that the molar tissue could continue to grow and cause heavier bleeding. There is also a small chance that the molar tissue could spread outside the womb. A definitive diagnosis is not made until the tissue removed has been examined in the laboratory.
For partial molar pregnancies it is unusual that the diagnosis is suspected on ultrasound scan and although you may have presented to hospital with bleeding you may have been diagnosed with a threatened or inevitable miscarriage and offered medical or surgical management of your miscarriage. The miscarriage tissue (if available) will always be sent to the laboratory for examination and it is only on laboratory examination that a diagnosis of a partial molar pregnancy is confirmed. Therefore, you will not know leaving the hospital that you may have a diagnosis of partial molar pregnancy and will only know when you are contacted and asked to return to the hospital for a blood test to check the pregnancy hormone level, called Human chorionic gonadotropin ( hCG)
Question: What happens if complete molar pregnancy (CHM) is suspected?
Answer: The pregnancy hormone hCG plays a very important role in the monitoring of the molar tissue cells as they produce high levels of hCG. If a complete mole (CHM) is suspected, it will be important for you to have a blood test to test the level of the pregnancy hormone hCG prior to a surgical procedure to empty the uterus of the abnormal tissue. This surgical procedure (called ERPC) will be performed as a day-case under general anaesthetic and the need for close follow-up will be explained to you. Following ERPC all patients will require close observation of their hCG levels (weekly). By monitoring the hCG levels your doctor will be able to identify if any of the molar tissue cells are still persisting.
Question: What happens before I leave the hospital if a complete molar pregnancy(CHM) is suspected?
Answer: It is important that the doctor discusses with you where you have your follow-up blood tests prior to discharge. You should get a full explanation of the probable diagnosis before you leave the hospital. You will receive this verbally from the doctor and the midwife will give you an information leaflet. The definitive diagnosis will be only be available after the laboratory has examined the miscarriage tissue and you should have an appointment to return to the hospital to discuss the diagnosis..
It is very important that you do not become pregnant until your follow-up is complete and you must take precautions against becoming pregnant during your follow-up. This is because a new pregnancy will produce hCG and it may be difficult for your doctor to determine if any of the molar cells are still present. You may use the oral contraceptive pill or use barrier methods for example condoms and one of these methods should begin immediately. However, you should not have a coil inserted until follow up is complete.
Question: Why is it important that I am followed up?
Answer: It is important that you are followed up after a molar pregnancy as these cells can remain in the uterus and potentially grow and spread. For your follow-up after a molar pregnancy it will be necessary for you to have regular blood tests to monitor the level of hCG in your blood. This is because molar tissue produces hCG. In Ireland we have established a National Centre for the monitoring of women diagnosed with molar pregnancy. This centre is called the National Gestational Trophoblastic Disease Registry, Monitoring and Advisory Centre and is located in Cork University Maternity Hospital under the leadership of Dr John Coulter.
Following diagnosis of a complete molar pregnancy (CHM) your hCG blood levels will be monitored on a weekly basis until the levels have returned to normal. This blood test can be performed at your local hospital or by your GP depending on your preference. Each result will be communicated to the National Gestational Trophoblastic Disease Registry, Monitoring and Advisory Centre at Cork University Maternity Hospital (CUMH) and you will be advised of the result of the test. In the vast majority of patients (85%) the hCG levels return to normal usually within 8 to 12 weeks. Following a normal result for 3 weeks in a row you will then have a blood test on a monthly basis for up to 6 months as there is a small risk that the cells can re-grow (recur). If all of these monthly results are normal, then your follow up will be complete and you will be discharged from the service.
In approximately 15% of patients the hCG levels will not return to normal, thereby signifying persistence of the complete molar cells. In these patients some chemotherapy treatment will be required to eliminate these cells. In the majority of cases (>95%) this chemotherapy treatment is successful in eliminating these cells.
Partial Molar pregnancy (PHM)
Following a diagnosis of a partial molar pregnancy your hCG blood levels will need to be monitored on a weekly basis until the levels have returned to normal. Once normal, only one further confirmatory blood test is required 4 weeks later. This blood test can be performed at your local hospital or by your GP depending on your preference. Each result will be communicated to the National Gestational Trophoblastic Disease Registry, Monitoring and Advisory Centre CUMH and you will be advised of the result and your progress. In approximately 98% of patients with a partial mole, the hCG levels will spontaneously drop to normal and no further treatment will be required, signifying that the molar pregnancy has resolved.
However, in 1-2% of patients the hCG levels do not return to normal and some chemotherapy treatment is necessary. In the majority of cases (>95%) this treatment is successful in eliminating these cells.
Becoming Pregnant Again
The majority of women with GTD who wish to will become pregnant again and have successful pregnancies. The risk of a further molar pregnancy is low. More than 98% of women who become pregnant following a molar pregnancy will not have a further hydatidiform mole and are not at increased risk of complications.
Risk of a repeat GTD
The risk of a repeat GTD is approximately 1 in 100, compared with approximately 1 in 600 risk in the general population.
Question: What is the National Gestational Trophoblastic Disease Registry, Monitoring and Advisory Centre?
Answer: The National Gestational Trophoblastic Disease Registry, Monitoring and Advisory Centre has been established to monitor and co-ordinate the follow–up and treatment of women who have had a molar pregnancy. The Centre is coordinated by the Health Service Executive, the National Cancer Control Programme and Cork University Maternity Hospital. It is located at Cork University Maternity Hospital and is the only such Centre in Ireland. After you have been diagnosed with a “Molar Pregnancy” it is very important that your doctor registers your details with us so that we can monitor and take care of you in the best possible way. Your agreement to this registration will be required.
The National Gestational Trophoblastic Disease Registry, Monitoring and Advisory Centre is managed by a team of specialist doctors, nurses and administrative staff. The information collected about patients is stored electronically in a secure server at CUMH and is only available to specific staff who will treat you and work directly with the Registry. The GTD Registry is governed by the provisions of the Data Protection Act 1988 (Amended 2003).